Abstract The onset of the COVID-19 pandemic in early 2020 has led to the publication of extensive guidance material to mitigate the spread of the virus indoors, including the management of HVAC systems. This review looks at Australia’s existing guidance on air quality in the healthcare sector and summarises the recent COVID-related recommendations from the major health authorities (CDC; CEC) and HVAC business associations (ASHRAE, REHVA, AIRAH). Several common themes emerge from this body of knowledge concerning improving ventilation, filtration, and novel air purification methods. These recommendations are directly applicable to the operators within the healthcare sector.
COVID-19 and the Role of Engineering Controls in Healthcare Settings
Hospital HVAC engineers may well be one of the unsung heroes of the COVID pandemic, as the knowledge of the airborne spread of the virus became widespread, and increasing demands were made for greater ventilation and/or filtration. Modifying the operation of mechanical systems to increase outside air intake or replacement of filters with higher performance specifications is no simple task. These activities, along with increasing vaccination rates and improved PPE have formed a key component in the fight against the SARS- COV2 virus (Figure 1).
Existing air quality standards in healthcare
Air quality standards for Australian healthcare facilities operate at a higher standard than equivalent buildings of equivalent scale/occupancy due to Infection Prevention and Control (IPC) priorities. The core documents establishing these standards are:
• Australasian Health Facility Guidelines Part D Infection Prevention and Control1
• Australian Standard publications AS 1668.2, Section 6 dealing specifically with mechanical ventilation of specific health care functions and
• Australian Standards Handbook 260 – Hospital Acquired Infections – Engineering Down the Risk
• State-specific design guidelines, particularly those issued by the Victorian Department of Health.
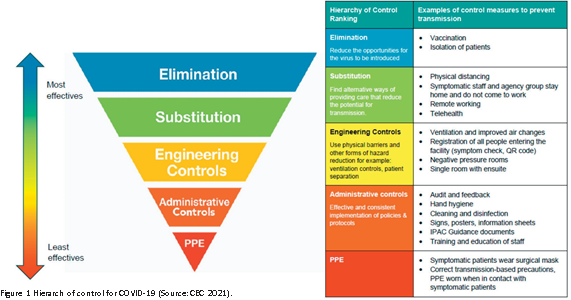
These requirements are summarised by the AIRAH publication DA15 Air Filters and Cleaning Devices – Selection and Application reproduced in Figure 2.
These standards, pre-date the emergence of COVID-19 and the pressure the disease has placed on
the healthcare sector around IPC outcomes. This review specifically examined whether healthcare authorities and the HVAC industry have formed any consensus around the appropriateness of current healthcare air quality standards.
1 https://aushfg-prod-com au.s3.amazonaws.com/Part%20D%20Whole_7_Nov%202020%20Reference%20Edit_1.pdf
The Victorian Health and Human Services Building Authority also issued “Engineering guidelines for healthcare facilities” in mid-2020 and these are discussed in more detail below.
What we know about COVID-19 – Virus Size and Dispersion as an Aerosol
The World Health Organisation (WHO) and the general healthcare sector were initially slow to recognise the airborne dispersal as the predominant vector for SARS-COV2 dispersal. Here in Australia and very early on in the pandemic, internationally recognised aerosol expert Professor Lidia Morawska and many others were warning about the IPC focus on near-field droplets and cleaning of surfaces (fomites). This paper also was very early in identifying ‘engineering controls targeting airborne transmission as part of an overall strategy to limit infection risk indoor’ and would include the very familiar themes of ensuring ‘sufficient and effective ventilation, possibly enhanced by particle filtration and air disinfection, avoiding air recirculation and avoiding overcrowding’. 2
2 Morawska, L., Tang, J. W., Bahnfleth, W., Bluyssen, P. M., Boerstra, A., Buonanno, G., Cao, J., Dancer, S., Floto, A., Franchimon, F., Haworth, C., Hogeling, J., Isaxon, C., Jimenez, J. L., Kurnitski, J., Li, Y., Loomans, M., Marks, G., Marr, L. C., Mazzarella, L., … Yao, M. (2020). How can airborne transmission of COVID-19 indoors be minimised?. Environment international, 142, 105832. https://doi.org/10.1016/j.envint.2020.105832
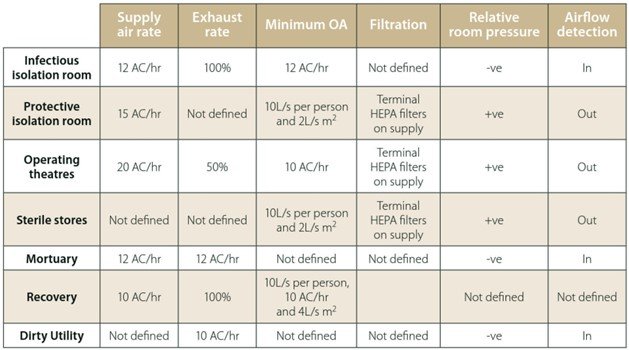
The SARS-CoV-2 virus is approximately 0.12 µm in size and is exhaled within a droplet as part of normal daily activities. Figure 3 shows the relative size of the virus and other common viruses in relation to human hair, PM2.5 and PM10 particles. The practical effect of exhaling particles of this size is visualised in Figure 4 with the ready spread of the virus within an inadequately ventilated space creating a risk of infection for others in the room over long distances and for an extended period. Engineering controls applied to this situation will not eliminate the risk of infection but can mitigate the likelihood of an infection occurring.
The best analogy for the movement of aerosols in a room is, as a non-smoker, being in the same room with a cigarette smoker. Cigarette smoke aerosols move within a room in a similar manner to virus particles and non-smokers in their proximity quickly become aware of their presence.

General COVID-19 Guidance for HVAC Engineers
There has been a very large volume of guidance material published relevant to the operation of HVAC systems in non-healthcare settings with the goal of diluting or entrapping airborne viruses to reduce transmission. Healthcare facilities already operate at standards significantly higher than general occupied buildings and it is not intended to review this guidance in detail. However, there are some excellent
online resources specifically targeted for Australian HVAC engineers:
AIRAH – Common questions about COVID-19 and air conditioning and refrigeration systems https://www.airah. org.au/AIRAH/Navigation/Industry_leadership/Coronavirus_information/Common_questions_about_COVID-19.aspx ;
A.G. Coombs – Modifying HVAC Systems to Reduce SARS-CoV-2 Transmission https://www.agcoombs.com. au/news-and-publications/advisory-notes/modifying-hvac- systems-to-reduce-sars-cov-2-transmission/.
| Title | Author | Ventilation | Filtration Novel Air Purification | Methods | Comment |
| Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic 1 | CDC Advisory | Optimize the Use of Engineering Controls and Indoor Air Quality: Explore options, in consultation with facility engineers, to improve ventilation delivery and indoor air quality in all shared spaces. | – | – | No reference to HVAC filtration or novel methods. |
| ASHRAE EPIDEMIC TASKFORCE – HEALTHCARE2 | ASHRAE | • Manage airflow from clean to less clean • Increased outside air fraction | Increase Filtration Level if Possible | Utilize portable anterooms with HEPA filtration UV air cleaning and upper air UV light can eradicate airborne SARS- CoV-2 virus | Published April 2021. |
| COVID-19 Infection Prevention and Control Manual3 | NSW Clinical Excellence Commission | High-risk patients should ideally be in a negative pressure room with anteroom. – A room with ≥12 air changes per hour (ACH) and controlled direction of airflow is recommended for Airborne Precautions – In a mechanically ventilated ‘airborne precaution room’ negative pressure (class N) is required to control the direction of airflow. | – | – | No reference to HVAC filtration or novel methods. Proposed standards are consistent with current standards summarised in Figure 2. |
| HVAC System Strategies to Airborne Infectious Outbreaks4 | Victorian Health and Human Services Building Authority | • Air handling systems should supply 100% outside air to controlled zones where capable or a maximum % of outside air. • Total air movement of between 150-200 l/s/double door into controlled zones • Modification to building HVAC system to ensure pressure differentials are maintained | Additional particle filtration in HVAC system is likely to reduce the airborne load of infections particles. Minimum filtration grade of MERV 13-16 (F8 or F9) advisable | Source capture filtration units can serve in high traffic areas UVGI systems can inactivate some disease-transmitting organisms | Published in November 2020 shortly following the release of the “Engineering guidelines for healthcare facilities – Vol 4”. |
1 https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
2 https://www.ashrae.org/file%20library/technical%20resources/covid-19/ashrae-healthcare-c19-guidance.pdf
3 https://www.cec.health.nsw.gov.au/ data/assets/pdf_file/0018/644004/COVID-19-IPAC-manual.pdf
4 https://www.vhba.vic.gov.au/engineering-guidelines-healthcare-facilities
The general guidance can be summarised as:
• Increase outdoor air ventilation to dilute indoor air and virus concentrations within the capacity of the HVAC system or, where available, utilising natural ventilation.
• Maintain a relative humidity between 40 and 60 percent to reduce virus survival times but ensure the body’s own mucous membrane functions properly as a defence mechanism.
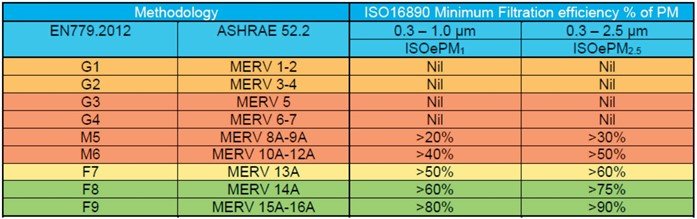
• Improve filtration to a minimum of a MERV13A (“A” implying filtration rating on a clean filter without reliance on any electrostatic charge and in accordance with ISO16890) within the capacity of the HVAC system. This would be equivalent to a PM1 50-60% filter under ISO16890 or an F7 filter under the superseded EN779:2012.
• Warn against novel technologies including ionisation, dry hydrogen peroxide, and chemical fogging/disinfection due to the absence of an established body of peer-reviewed evidence showing proven efficacy and safety under as-used conditions.
• Application of UV treatments that are engineered correctly and properly maintained.
Health Sector-Specific Guidance
While several publications have addressed control measures to limit the spread of COVID-19 in the healthcare sector, a number of these deal exclusively with PPE only, and do not address other engineering control measures such as HVAC management. Table 1 summarises key findings of recent publications by the US Centre for Disease Control (CDC), American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE), the NSW Clinical Excellence Commission (CEC), and the Victorian Health and Human Services Building Authority (VHHSBA). The VHHSBA publication is notable in that it specifically relates to HVAC management strategies in the Australian healthcare sector and builds on the mid-2020 VHHSBA publication
“Engineering guidelines for healthcare facilities: Volume 4 – Heating, ventilation and air conditioning – Health technical guideline HTG-2020-004”3. These HVAC design parameters draw heavily on the AHSRAE Standard #10 published in 2017 entitled “Ventilation of Health Care Facilities” and contains far more detailed design parameters for healthcare facility systems calculated in terms of minimum ACH and outdoor air supply.
Discussion of key themes to emerge from published COVID-19 guidance
Healthcare facilities should seek to modify their HVAC systems to dilute and/or entrap airborne viruses to reduce the potential for disease transmission. Depending on the HVAC system in question, these modifications can be complex and require specialist advice to ensure system performance and balancing.
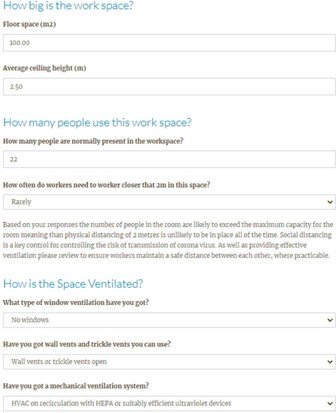
Risk Assessment Tools for Ventilation Adequacy
In terms of undertaking your own risk assessment of indoor spaces, there are several free tools available to determine the adequacy of ventilation based on room size, occupancy, and methods of ventilation. These tools require no specific expertise or training and provide an effective rule of thumb
whether additional control measures are necessary (Figure 5).
Using CO2 as a proxy measure of ventilation adequacy/disease risk
Measurement of CO2 concentrations in a fully occupied indoor space is cheap to measure and a useful proxy for the adequacy of existing mechanical or natural ventilation. This method does have its limitations, however, as the adequacy of the ventilation needs to be tested when the room is at maximum occupancy for an extended period. This suggests the use of permanently installed CO2 monitors as a key measure for assessing the adequacy of ventilation indoors. A recent AIRAH/REHVA publication recommends an orange light indicator at 800 ppm and a red-light indicator at 1,000 ppm as appropriate standards for Australian schools.4
3 Retrieved from: https://www.vhba.vic.gov.au/engineering-guidelines- healthcare-facilities
4 Retrieved from: https://www.rehva.eu/fileadmin/user_upload/REHVA_ COVID-19_Guidance_School_Buildings.pdf
1 Retrieved from: https://www.ashrae.org/technical-resources/filtration-disinfection#mechanical
1 Wladyslaw Kowalski (2003) cited in PA Jensen. Use of Ultraviolet Germicidal Irradiation as a Control to Limit Airborne Transmission. ACGIH eLearning Presentation, 10 June 2020

Filtration of Recirculated Air in HVAC Systems
The generic guidance published by AIRAH and ASHRAE recommends minimum filtration standards of MERV13 on recirculated air or a combination of filters that can achieve this target. In most healthcare settings, filtration meet this standard with the VHHSBA’s Engineering Guidelines for Healthcare Facilities recommending MERV 13-16 (F8 or F9) for in-patient settings (Table 2).
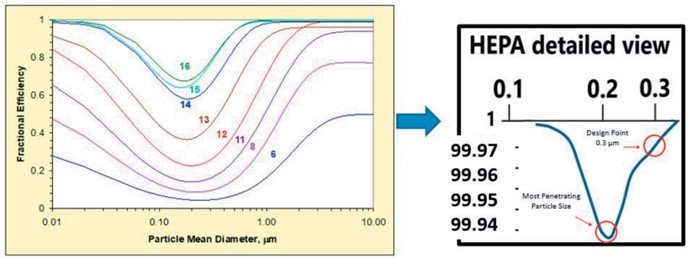
Many other specialist healthcare zones utilise HEPA (High-Efficiency Particulate Air) filtration in protective isolation rooms, operating theatres, and sterile stores. HEPA efficiency is higher than MERV16/F9 and removes at least 99.97% of dust, pollen, mould, bacteria, and any airborne particles with a size of 0.3 μm (Figure 6).
Alternative air cleaning options – UVGI and Portable Air Cleaners
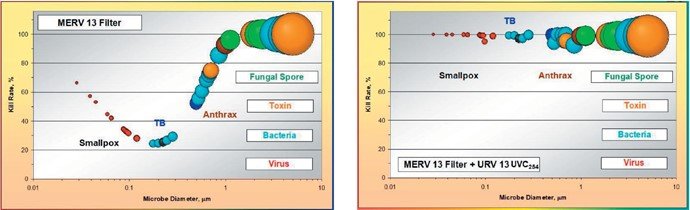
In many critical healthcare situations, the HVAC system capacity cannot accommodate the pressure differences associated with higher efficiency filters. In these circumstances, ASHRAE recommends a combined air cleaning option utilising filtration and ultra-violet germicidal irradiation as a means of increasing equivalent ACH and accommodating limitations of the HVAC system.5 Due
to the relatively low fractional efficiency of MERV filters in the 0.10 – 0.3 µm size range, often a combination of filtration and UVGI can result in HEPA-equivalent elimination of pathogens (Figure 7). COVID-19 and coronaviruses are known to be highly susceptible to UVGI (Kowalski, 2009).6
Portable air cleaners are stand-alone devices with a fan drawing air through a HEPA filter. The University of Melbourne provides an online comparison tool for HEPA-filtered portable air cleaners and comparing unit costs with the clean air delivery rate.
Conclusion
This article aims to identify the key recommendations relevant to reducing the risk of COVID-19 spread through hospital HVAC systems. The application of recommended control measures may be constrained by limitations on the existing HVAC systems. Any major changes to outside air utilisation and/or reuse of return air will likely require major system modifications and specialise mechanical engineering advice. Portable cleaners and UVC technology can provide solutions for limitations on the HVAC system, but specialist advice should be sought in assessing these options. Similarly, the use of CO2 monitors and risk assessment of indoor spaces should also be done by a qualified occupational hygienist or indoor air expert.
About the Author
Gregor Riese is a Director of Opira who provide specialist indoor air risk management products and services to the healthcare sector. Gregor is a qualified occupational hygienist based in Sydney.
5 ASHRAE Source: https://www.ashrae.org/file%20library/technical%20 resources/covid-19/ashrae-filtration_disinfection-c19-guidance.pdf
6 Wladyslaw Kowalski (2009) Ultraviolet Germicidal Irradiation Handbook – UVGI for Air and Surface Disinfection. Springer Berlin Heidelberg.